Our Solution
To pump effectively the billions of individual heart muscle cells are coordinated by the organised flow of electricity through the heart. Heart electrical activity is governed by a property of cardiac muscle cells called restitution. This property controls the amount of time that the individual muscle cells spend contracting and relaxing.
 LifeMap measures the restitution properties of the heart. It then creates an electrical instability map by measuring regional differences in restitution. LifeMap does this using electrical signals recorded from the body surface.
LifeMap measures the restitution properties of the heart. It then creates an electrical instability map by measuring regional differences in restitution. LifeMap does this using electrical signals recorded from the body surface.
LifeMap has won a series of awards both for its commercial potential and for the high quality scientific research that underpins it.
How to do a LifeMap test?
Living with a condition that carries a risk of sudden cardiac death is like being in an earthquake zone. There is a constant unpredictable risk of disaster. A LifeMap test works by listening to the heart’s electrical activity and using this to accurately predict the earthquake so that the risk can be appropriately managed. At present LifeMap is a minimally invasive Electrophysiology test. Electrophysiology tests have been part of routine heart investigations for over 30 years and are done every day in hospitals worldwide.
Minimally Invasive
The electrical signals for a LifeMap test are acquired using a very simple Electrophysiology test that could be done by any Cardiologist. An invasive LifeMap test takes 5 minutes and is a very low risk procedure which is done under local anaesthetic. A pacing wire is passed to the heart through a tiny hole in the vein in the leg. The wire is then used to pace the heart for five minutes, this is completely painless. The wire is taken out and the test is finished.
Exercise LifeMap
The science behind LifeMap requires a spectrum of heart rates to analyse electrical instability. The initial research achieved this with an electrophysiology test. The ULTIMATE study investigated using exercise or isoprenaline (a drug that increases heart rate) to produce a spread of heart rates. The ULTIMATE study has completed recruitment and currently endpoints are being analysed, preliminary data is promising.
The Evidence for LifeMap
For research papers LifeMap has been termed the Regional Restitution Instability Index (R2I2) and the Peak Electrical Resitution Slope (PERS).
A summary of the development of LifeMap has been published in EP Europace.
The precise mechanisms by which the heart becomes electrically unstable and sudden cardiac death happens have been the subject of intensive research for a century. We have taken this understanding and added to it at the University of Leicester with a decade of ground breaking sudden cardiac death research. LifeMap is a culmination of this work and brings what we have learnt to the bedside.
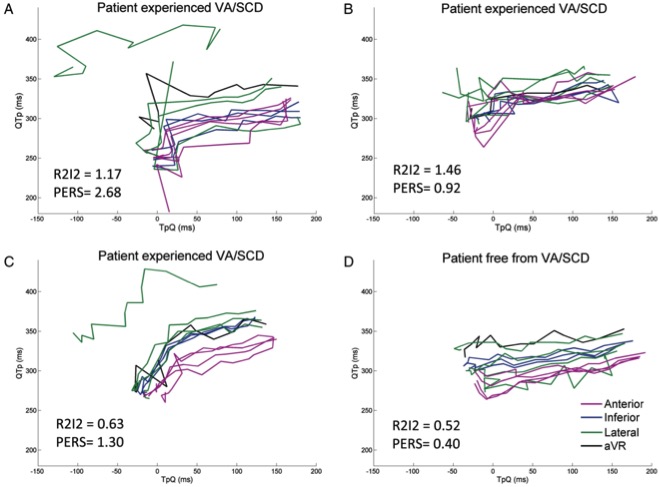
Clinical studies of LifeMap have been performed on seven different cohorts of patients. LifeMap has been consistently shown to effectively identify patients at risk of sudden cardiac death. LifeMap quantifies risk of sudden cardiac death by two key techniques, first by measuring regional differences in restitution gradient and secondly by measuring the average peak restitution gradient. LifeMap produces two numbers that are directly proportional to a person’s risk of sudden cardiac death.
LifeMaps for two patients with ischaemic heart disease causing weakness of the heart muscle
LifeMap has been presented at and has won research prizes at numerous International Cardiology Conferences including Heart Rhythm Annual Scientific Sessions, European Society of Cardiology, American Heart Association’s Scientific Sessions, Heart Rhythm Congress, European Heart Rhythm Association Congress and CardioRhythm.
Clinical Study 1
A Novel Surface Electrocardiogram Based Marker of Ventricular Arrhythmia Risk in Patients with Ischemic Cardiomyopathy
Our first study looked at LifeMap (R2I2) in normal controls and retrospectively in two groups of people with Ischaemic heart disease. In America alone, each year 1.5 million people present with Ischaemic heart disease and experience a myocardial infarction.
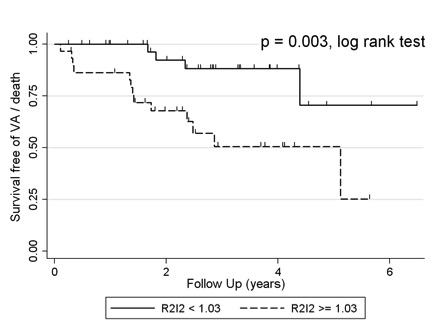
R2I2 was found to be significantly higher in patients experiencing ventricular arrhythmia or death in both cohorts of patients with Ischaemic heart disease. R2I2 was independent of standard risk markers in predicting ventricular arrhythmia or death. R2I2 was significantly lower in control patients than in patients at risk of sudden cardiac death.
Clinical Study 2– ICD-IRS
Prospective evaluation of two novel ECG-based restitution biomarkers for prediction of sudden cardiac death risk in ischaemic cardiomyopathy
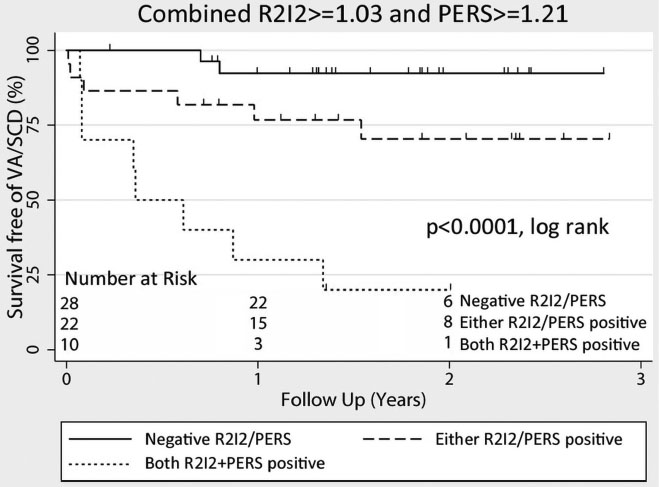
Our next study repeated the first study prospectively. The aim was to replicate the previous study and to show that LifeMap (R2I2), using the predefined technique and cut-off value, was effective at predicting risk of sudden cardiac death.
Patients positive for both R2I2 and PERS had a relative risk of ventricular arrhythmia / sudden cardiac death more than 21 times greater than that of patients negative for both risk markers. R2I2 and PERS were highly effective in separating out patients with ischaemic heart disease into high and low risk groups. Again, R2I2 and PERS were independent of existing risk markers in predicting risk of sudden cardiac death.




